AquilaEHR Helps Practices Stay Up-To-Date on MIPS Quality Payment Programs (QPP)
MACRA is the Medicare Access and CHIP Reauthorization Act. MACRA replaces the current Medicare reimbursement schedule with a new pay-for-performance program that’s focused on quality, value, and accountability.
According to the Centers for Medicare and Medicaid Services (CMS), MACRA introduces a new payment system that compensates healthcare providers for providing higher-quality care rather than more services.
On April 16, 2015, President Obama authorized the Medicare Access and CHIP Reauthorization Act (MACRA). The House of Representatives voted it through 392 to 37, while the Senate approved it 92 to 8. Its bipartisanship is a proof of MACRA’s legislative support and demonstrates its importance in the country’s healthcare reform.
Merit-based Incentive Payment System, or “MIPS,” is the result of MACRA’s integration of the Physician Quality Reporting System (PQRS), Value-based Payment Modifier (VBM), and the Medicare Electronic Health Record (EHR) incentive programmer.
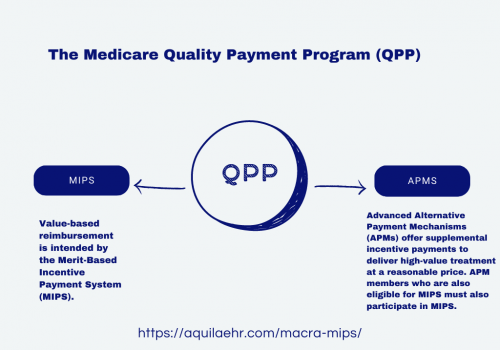
MIPS → Merit-based Incentive Payment System
Value-based reimbursement is intended by the Merit-Based Incentive Payment System (MIPS).
APMS → Alternative Payment Model
Advanced Alternative Payment Mechanisms (APMs) offer supplemental incentive payments to deliver high-value treatment at a reasonable price. APM members who are also eligible for MIPS must also participate in MIPS.
Merit-based Incentive Payment System
The Physician Quality Reporting System (PQRS), the Value-based Payment Modifier (VBM), and the Medicare Electronic Health Record (EHR) Incentive Program are combined into the Merit-Based Incentive Payment System, which measures Eligible Professionals (EPs) in four areas:
1. Quality 2. Cost
3. Improvement Activities4. Promoting Interoperability (formerly Meaningful Use of certified EHR technology)
Alternative Payment Model
Advanced Alternative Payment Mechanisms (APMs) offer supplemental incentive payments to deliver high-value treatment at a reasonable price. APM members who are also eligible for MIPS must also participate in MIPS.
Although the CMS is presently defining alternative payment methods, some Accountable Care Organizations (ACOs), Patient Centered Medical Homes, and bundled payment models will be examples. Although CMS has suggested these as potentially qualifying for APMs, providers are not automatically eligible for an APM by taking part in those models.
Eligibility Criteria
- Surpass the low-volume limit as an individual or a group.
- Enrolled in the Medicare before 2020.
- Do not become a Qualified Participant (QP) or even a Partial QP.
- An APM individual with QP status wishes to participate in MIPS.
- Are part of an APM Entity MIPS APM entity that exceeds the low-volume threshold.
Find out more about how to determine your eligibility
All eligible healthcare professionals must participate in MIPS. Check your participation status
To earn more, Improve your MIPS Score
MIPS allows physicians to receive a better performance-based payment adjustment on reimbursements based on their reporting score. So, let AquilaEHR help earn you more as you document and keep track of your performance towards achieving your MIPS objectives.
Quality (45%)
Replacing PQRS, this category focuses on the quality of care you deliver, based on CMS performance measures as well as stakeholders and other medical professionals. You can pick six measures of performance that best suit your practice.
Promoting Interoperability (25%)
This category covers patient engagement as well as the use of Certified Electronic Health Record Technology (CEHRT) during exchange of information. This is done by actively sharing information in a comprehensive manner with patients and other clinicians. These include sharing visit summaries, therapeutic plans and test results with patients and other facilities.
Improvement Activities (15%)
A relatively new category, this is used to measure your participation in improvement of your practice. This includes activities that can improve your patient engagement, increase access to care. You are allowed to choose activities that better suit your practice such as patient and clinical shared decision-making, expansion of practice access and enhancing care coordination.
Cost Measures (15%)
This category replaces VBM. The cost of the care you provide to patients based on your Medicare claims is calculated by CMS. MIPS measures the total cost care throughout the year or during a patient’s hospital stay.


